For patients with long-term multiple missing teeth, the goal is often simple—but difficult to achieve: walk out with fixed teeth quickly, regain chewing efficiency, and restore a natural smile, all while keeping surgery and appointments to a minimum. This case demonstrates how a fully digital workflow—combined with chairside zirconia fabrication using the UP3D P55D in the definitive stage—can help deliver a predictable, time-efficient full-arch rehabilitation and complete functional and esthetic reconstruction within three months.
This case was completed by visiting clinicians Dr. Huang and Dr. Wang under the supervision of Dr. Zhong. All clinical records and images are shared with the patient's informed consent.
1. Patient Overview
-
Patient: Ms. M., female, 44 years old
-
Chief complaint: Long-standing multiple missing teeth in both arches, affecting mastication and appearance
-
History of present illness: Multiple teeth were lost years ago. The patient previously wore a removable denture but could not tolerate it long term.
-
Medical history: Generally healthy; no known systemic disease, drug allergies, or history of infectious disease
-
Treatment expectations: Minimal trauma, lower cost, fewer visits, a shorter treatment timeline, and rapid recovery of dentition and chewing function
2. Pre-Operative Examination and Analysis
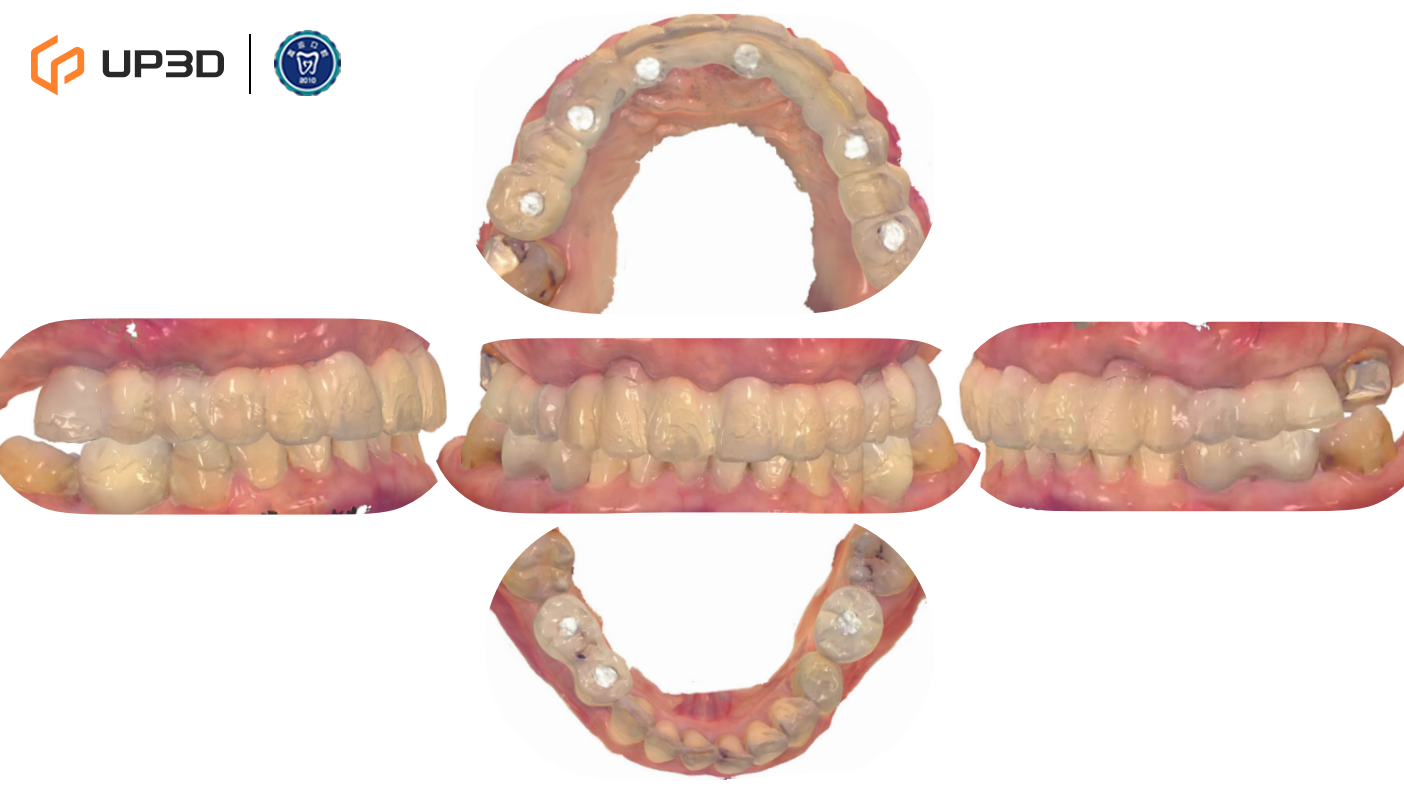
2.1 Intraoral Findings and Intraoral Scan Assessment


A digital intraoral scan (IOS) was used to capture maxillary and mandibular models. Clinical findings included multiple missing teeth, disordered dentition, and occlusal collapse with reduced facial support. Bone volume was limited in certain regions. The 3D scan clearly presented tooth morphology, soft tissue contours, and occlusal relationships—providing accurate data for subsequent digital implant planning.
2.2 Facial Analysis

Frontal and profile photographs showed reduced lower facial height, inadequate facial support, and an unbalanced smile line. As the patient traveled for treatment, she strongly preferred an “immediate teeth” solution with minimal trauma, lower cost, and a shortened timeline.
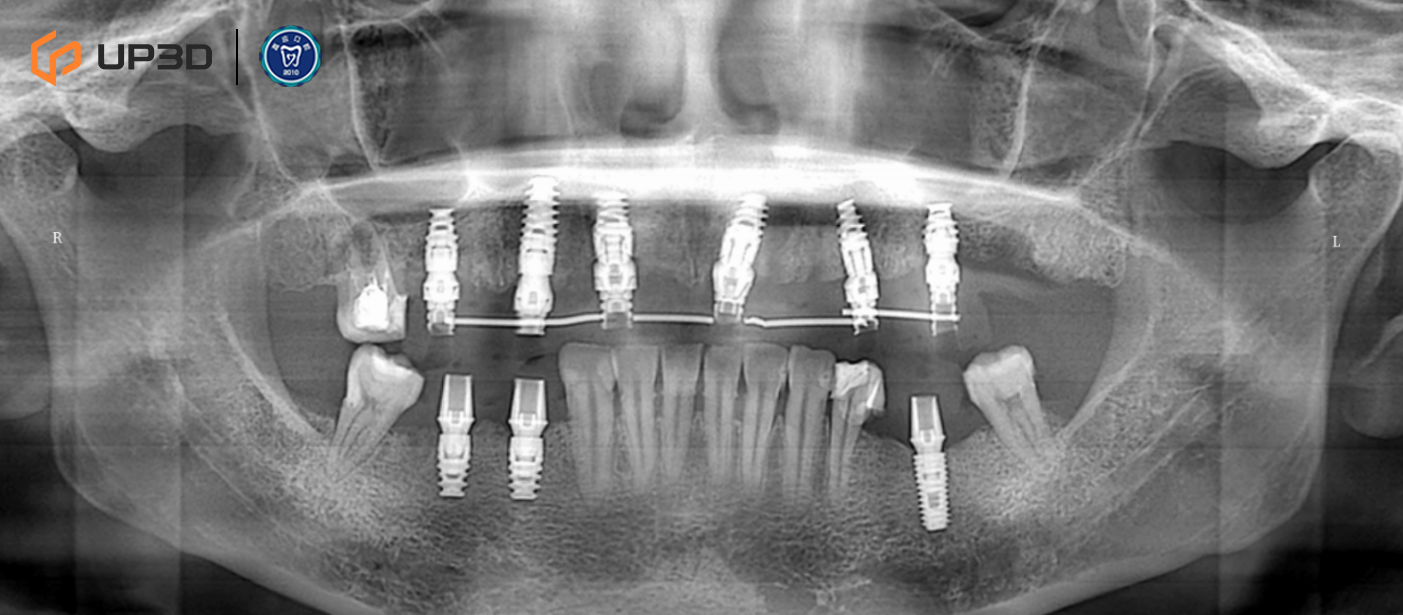
2.3 Radiographic Assessment
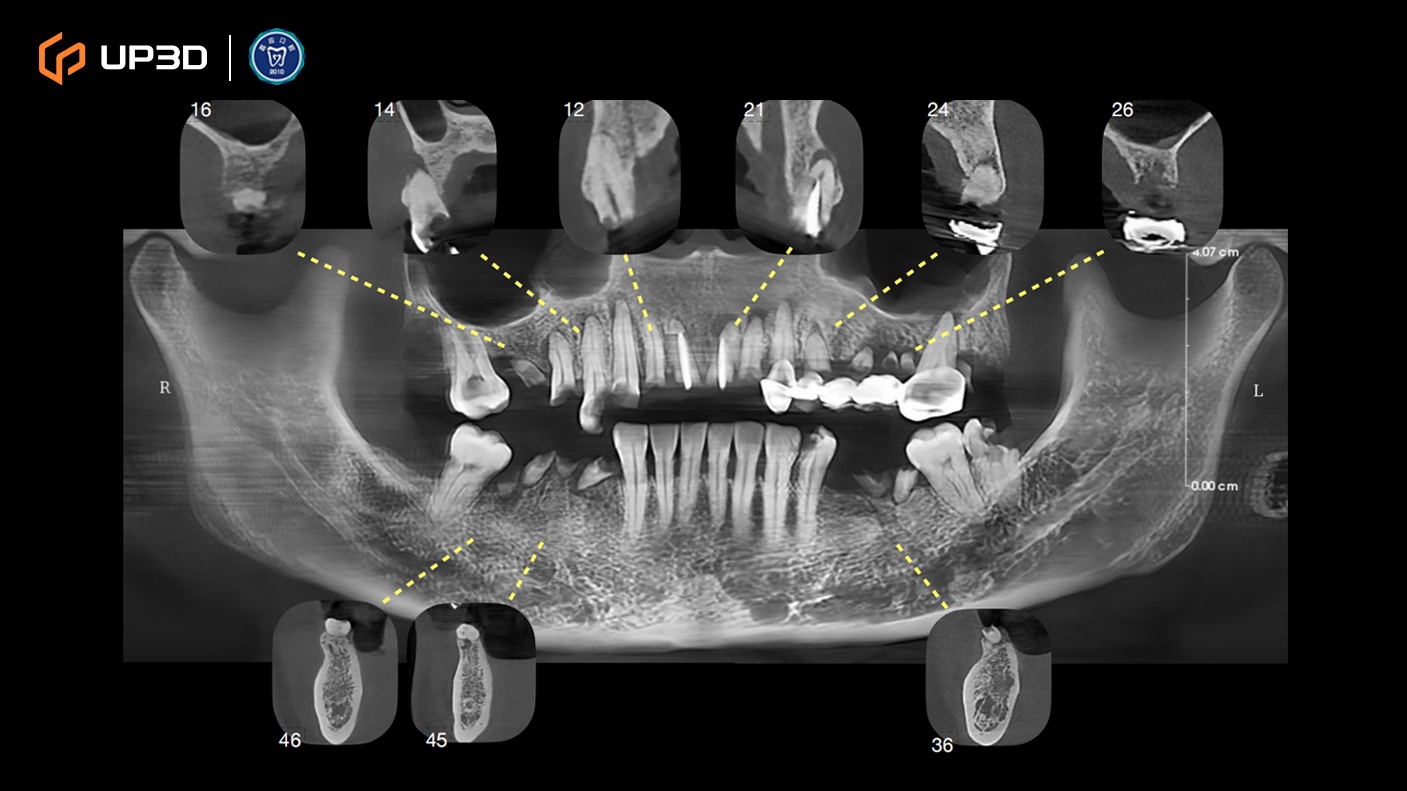
A panoramic radiograph and cone-beam computed tomography (CBCT) revealed multiple missing teeth and uneven alveolar ridge resorption, with moderate-to-limited bone volume in selected areas. Based on measurement and analysis, implant placement was planned at sites including 16, 14, 12, 21, 24, 26, 36, 45, and 46 (FDI tooth numbering).
3. Digital Diagnosis and Treatment Planning
3.1 Integrated 3D Planning
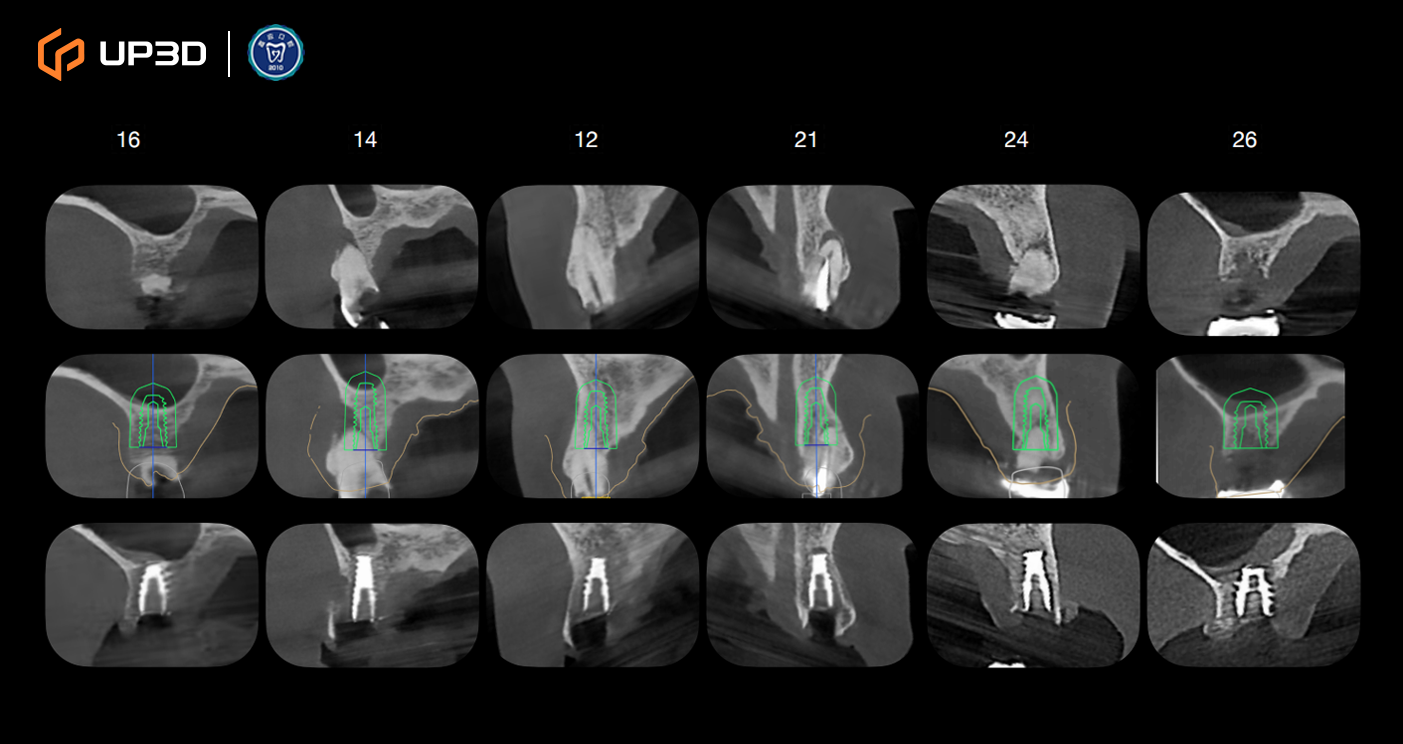
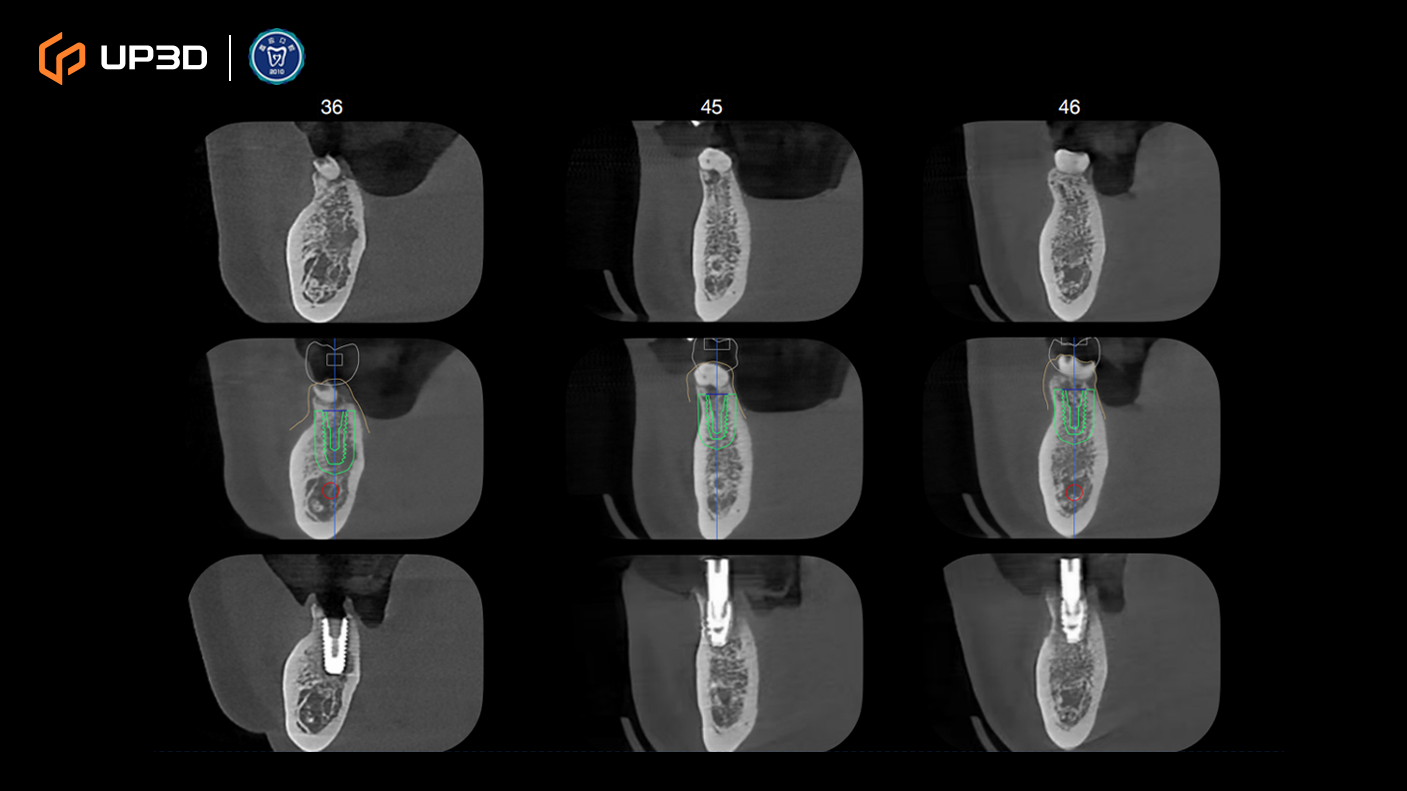
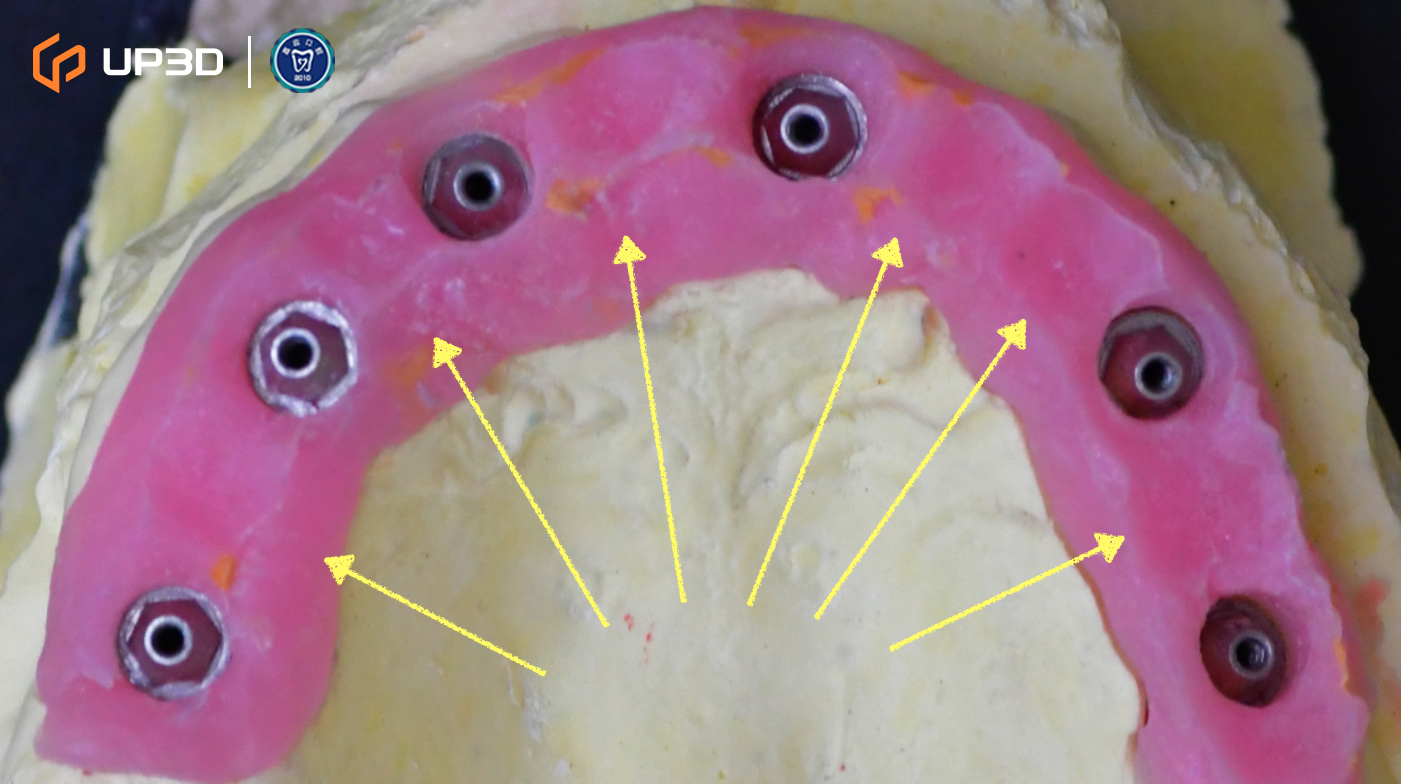
Intraoral scan data were merged with CBCT to complete a 3D implant plan:
-
Six implants planned in the maxilla and three implants in the mandible
-
Surgical guide (guided surgery) pathways were planned digitally
-
Digital tooth setup and guide fabrication supported accurate positioning and a minimally invasive approach
Guided surgery helped improve consistency in implant angulation and depth control, supporting a stable foundation for immediate loading.
4. Immediate Restoration Workflow
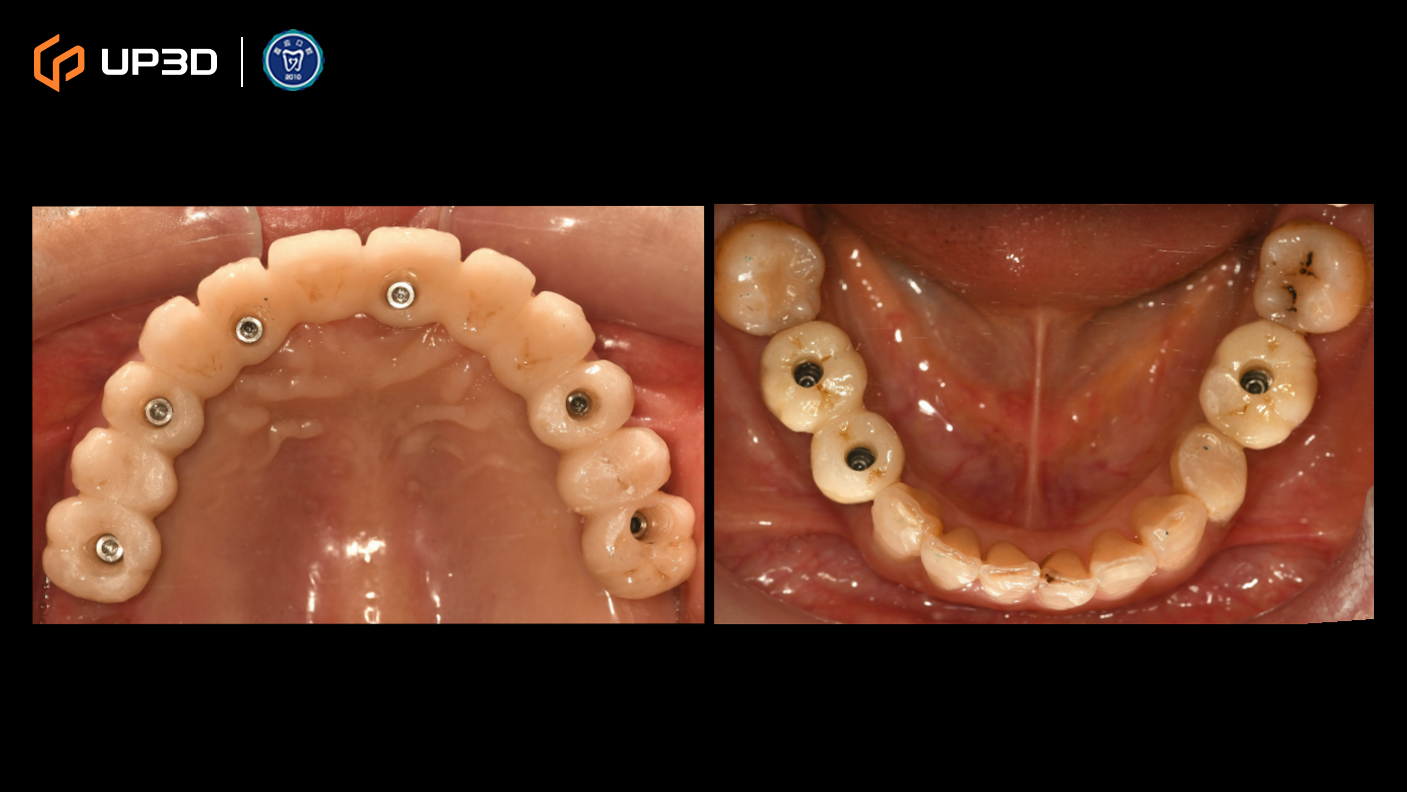
4.1 Scan Body Placement
After implant placement, scan bodies were installed to ensure accurate transfer of implant positions to the digital workflow.
4.2 Intraoral Scanning (Digital Impression)
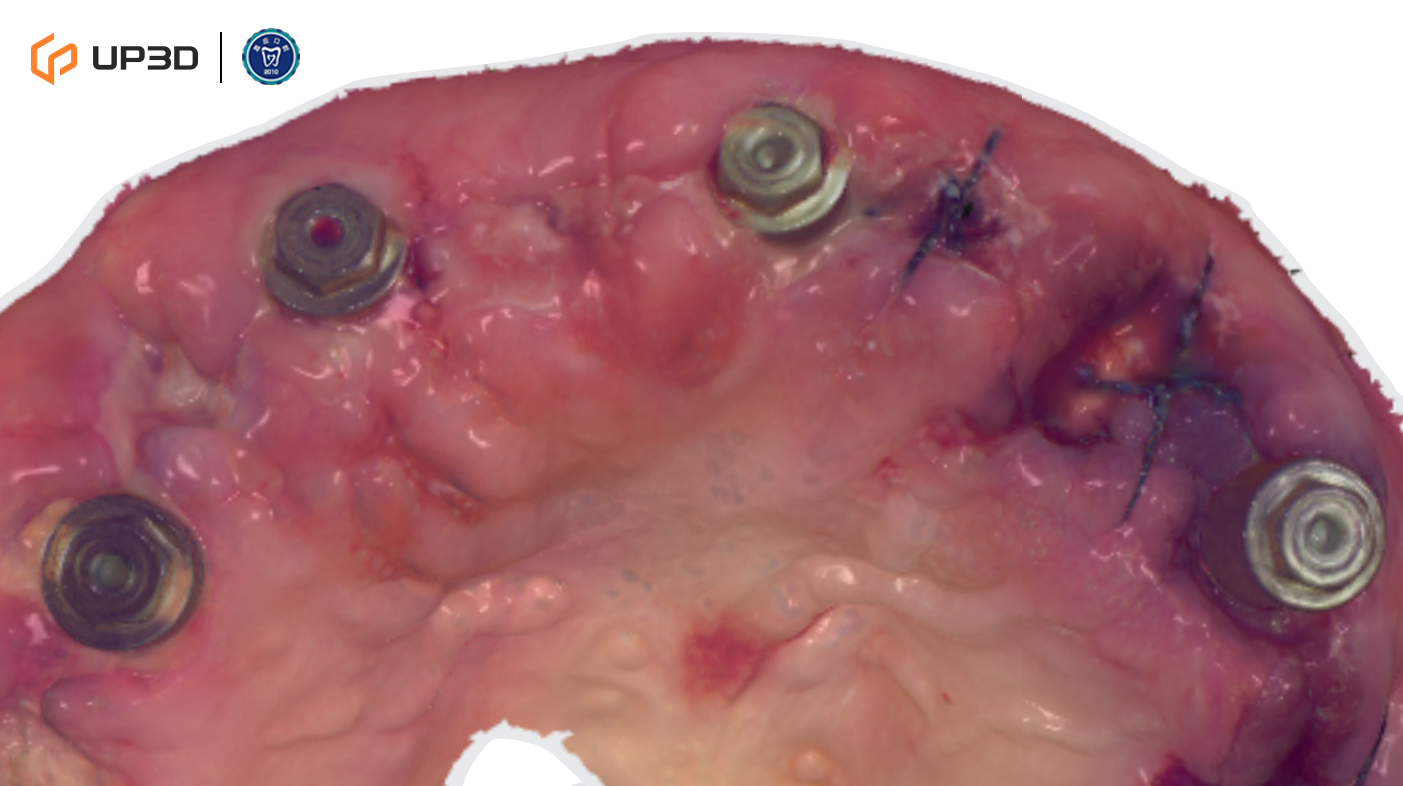
Intraoral scanning was performed chairside to capture soft tissue contours and implant positions, providing the dataset for designing an immediate provisional restoration.
4.3 Design and Fabrication of the Immediate Provisional Restoration
-
CAD software was used to design the immediate provisional prosthesis
-
A chairside milling unit was used to fabricate the restoration from a resilient resin disc material
-
The prosthesis was designed to be lightweight, with balanced stress distribution and appropriate occlusal contacts
5. Immediate Loading Phase
5.1 Delivery and Occlusal Reconstruction
The immediate provisional prosthesis was delivered chairside post-operatively, followed by occlusal reconstruction and initial adjustments. The patient regained esthetics and basic chewing function immediately, reporting good comfort.
5.2 Six-Week Follow-Up
Follow-up evaluation showed a mean Implant Stability Quotient (ISQ) ≥ 75, indicating favorable stability and suitability for continued loading.
6. Stabilized Provisional Phase
6.1 Ongoing Adjustment and Occlusal Optimization

Before the definitive restoration, the stabilized provisional prosthesis was worn for an additional six weeks for observation and fine-tuning:
-
Evaluation of occlusal contacts, phonetics, and hygiene access
-
Confirmation of healthy soft tissue healing and stable contours
6.2 Soft Tissue Conditioning
Soft tissue contours were guided by the prosthesis margins to establish a natural-looking transition and a more favorable emergence profile.
7. Definitive Restoration Phase
7.1 1:1 Digital Duplication of the Stabilized Provisional

After verifying the stabilized provisional’s morphology and occlusion clinically, a 1:1 digital duplication was performed to ensure the definitive prosthesis closely replicated the validated provisional stage.
7.2 Digital Scan Transfer and CAD/CAM Nesting
Scan data were used to replicate the stabilized provisional and complete CAD/CAM nesting and design, supporting accuracy and traceability throughout the workflow.
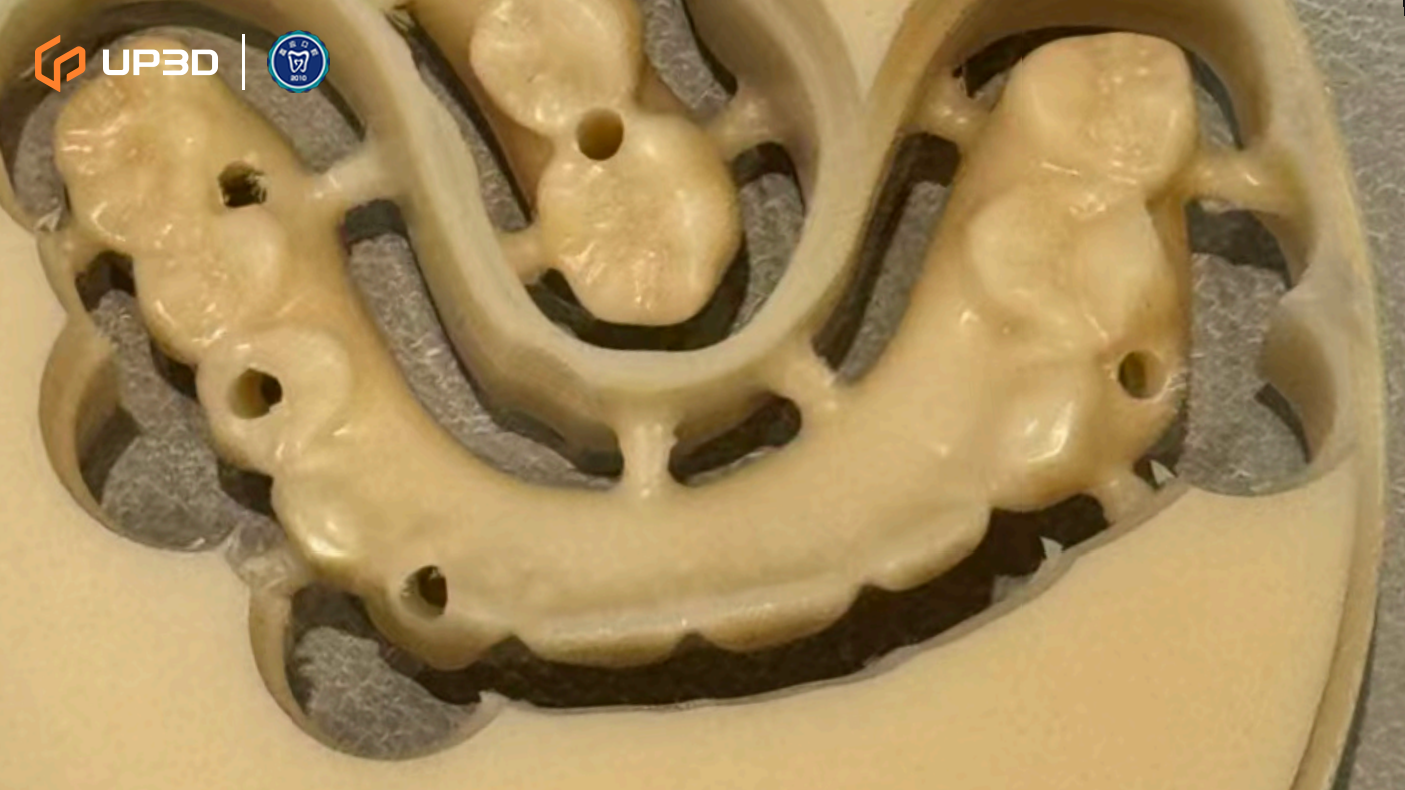
7.3 Chairside Milling of the Zirconia Restoration

High-strength zirconia was selected for chairside fabrication. Milling was performed using the UP3D P55D. The definitive restorations showed:
-
Clean, well-defined margins that supported accurate seating
-
Stable surface quality and consistent milling results
-
High fidelity in anatomical morphology and occlusal detail reproduction—helping reduce chairside adjustments and minimizing the risk of remakes
The zirconia restorations were completed within approximately 48 hours, enabling a timely transition into final delivery.
7.4 Final Delivery

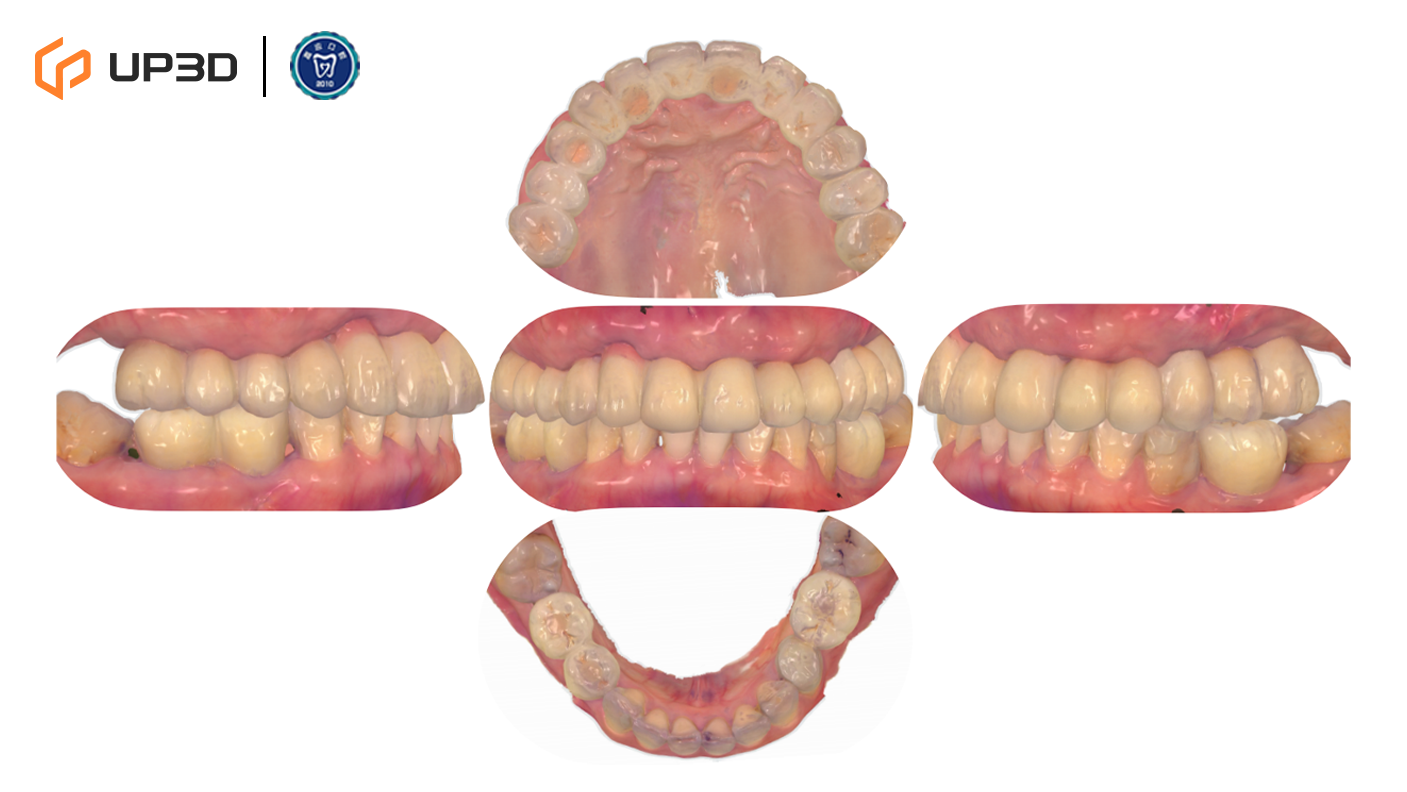
After delivery, the definitive prosthesis demonstrated:
-
Balanced occlusal contacts and an esthetically pleasing profile
-
Appropriate hygiene access and comfortable function
-
A post-delivery intraoral scan was archived to establish a digital record for future comparison and maintenance
8. Outcome and Follow-Up
8.1 Post-Delivery Facial and Smile Evaluation




Frontal and profile photographs indicated:
-
Improved lower facial support and a more natural smile line
-
A more relaxed expression and improved facial proportions
-
High patient satisfaction with both esthetics and function
8.2 Three-Month Follow-Up


-
Panoramic imaging showed stable implant and prosthesis positioning
-
Occlusion remained stable, with no evident peri-implant bone changes on follow-up imaging
-
The staged rehabilitation was completed successfully as planned









